Introduction: The Foundation of Facial Aesthetics 🤓
In the pursuit of a strong, defined facial structure, attention often focuses on superficial elements like skin, muscle tone, and fat percentage.
However, the true foundation of facial aesthetics—the underlying skeletal framework—is frequently overlooked.
Facial bone mass and density, particularly in the mandible (jawbone) and zygomatic arches (cheekbones), are the ultimate determinants of a chiseled, youthful, and robust appearance.
As we age, bone resorption—the natural process of bone breakdown—can lead to a loss of facial volume, contributing to sagging skin and a less defined profile.
While professional measurement of bone mass requires advanced medical imaging like DEXA scans or Cone-Beam CT (CBCT), these are not accessible for routine, at-home assessment.
The question then becomes: How can an individual non-invasively and indirectly gauge the health and mass of their facial bones from the comfort of their home?
This comprehensive guide will explore the scientific principles of facial bone health and provide actionable, indirect methods you can use to assess your craniofacial structure.

The Science of Facial Bone Health: Why It Matters 🧬
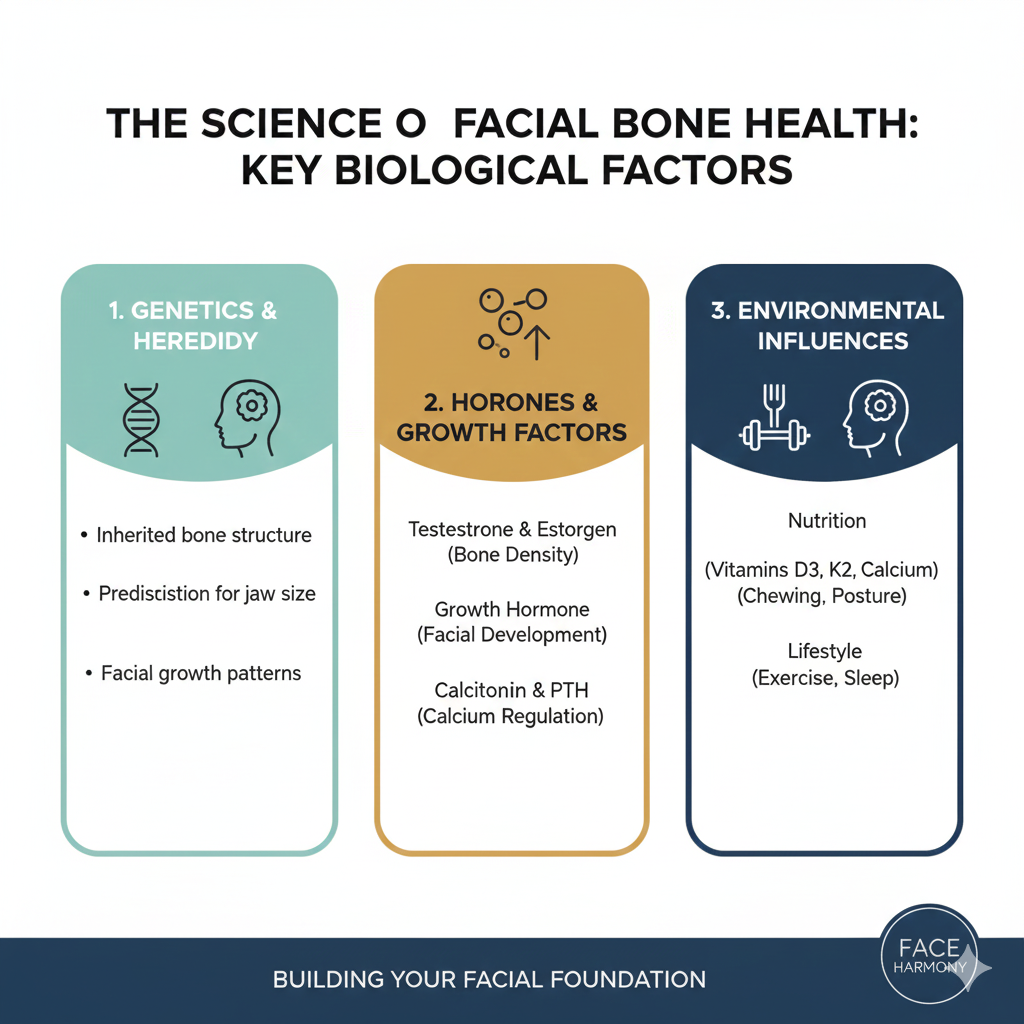
Unlike the long bones of the arms and legs, the bones of the face—the maxilla, mandible, and zygoma—are constantly subjected to forces from chewing, speaking, and even breathing.
This constant mechanical stress is crucial because bone is a living tissue that responds to load.
The principle of Wolff’s Law states that bone tissue will adapt to the loads under which it is placed.
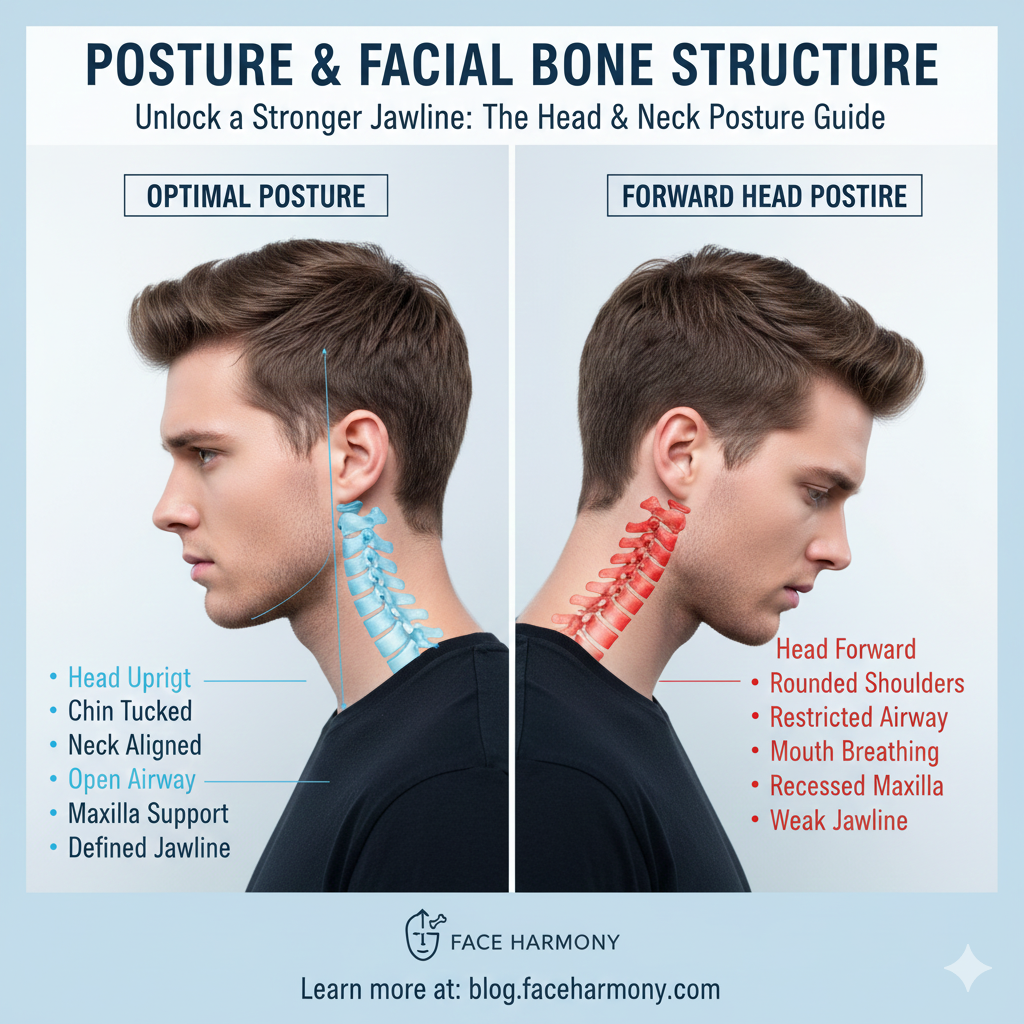
In the face, this means that proper chewing, correct tongue posture, and nasal breathing all contribute to maintaining and even increasing bone density and mass.
Conversely, a lack of mechanical stimulation, such as a soft diet or mouth breathing, can lead to bone atrophy, particularly in the alveolar bone that supports the teeth.
Furthermore, facial bone mass is intrinsically linked to systemic bone health.
Conditions like osteoporosis, which is a decrease in bone mineral density, often manifest in the jawbone before other areas, making it a critical indicator of overall skeletal health Jawbone Density and Osteoporosis.
The health of your facial bones is not merely an aesthetic concern; it is a vital component of your overall physiological well-being, affecting everything from airway function to dental stability.
Method 1: The Anthropometric Proxy—Measuring Bone Projection 📐
Since direct measurement of bone density is impossible at home, we must rely on anthropometric proxies—measurements of the soft tissue that closely reflect the underlying bone structure.
The most effective proxy for facial bone mass is the measurement of bone projection and width, which can be done with simple tools like a caliper or a ruler and a mirror.
A. Mandibular Width and Projection (Jawbone Mass)
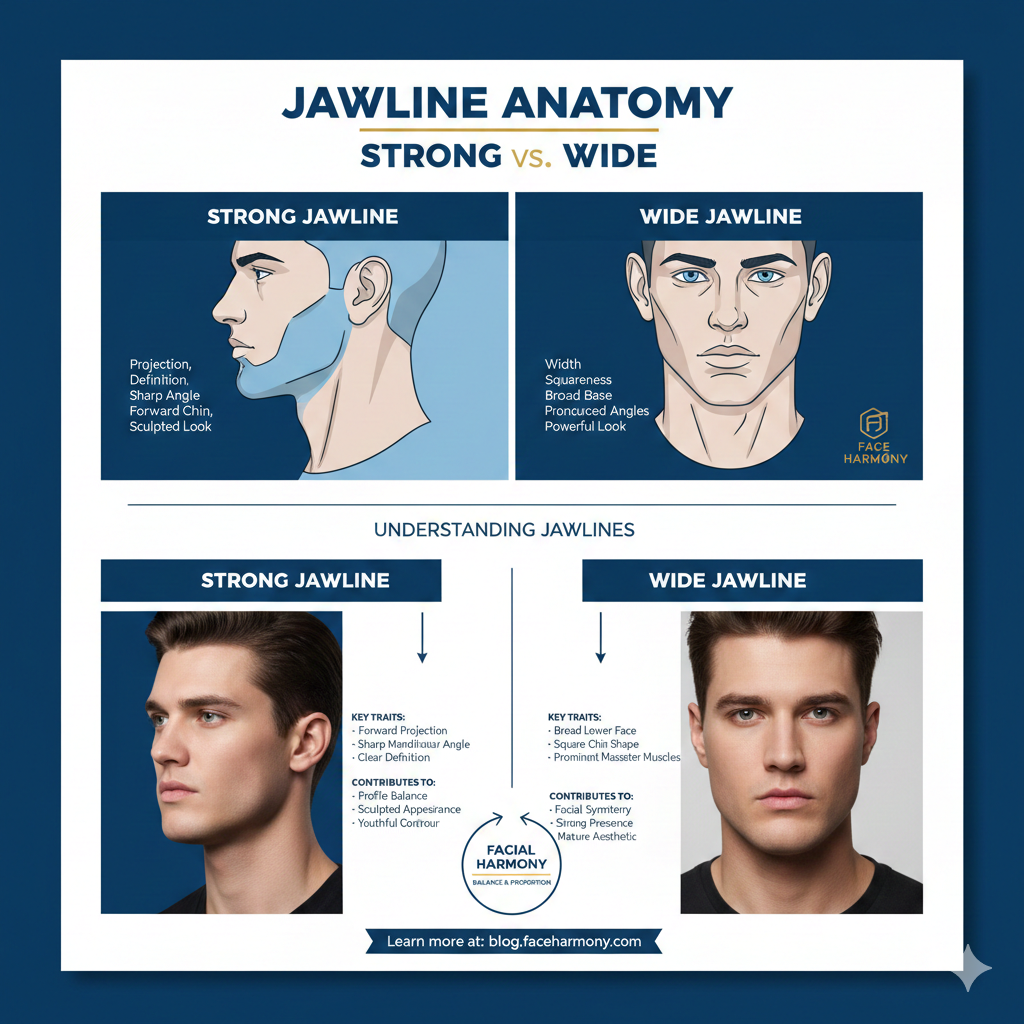
A strong jawline is a direct reflection of a robust mandible.
To indirectly assess the mass of your jawbone, focus on the following measurements:
- Bigonial Width: The distance between the most lateral points of the mandibular angles (the corners of your jaw). A wider bigonial width is a strong indicator of a larger, more massive mandible.
- Gonial Angle: The angle formed by the intersection of the lower border of the mandible and the posterior border of the ramus. A sharper, more acute angle (closer to 90-110 degrees) is associated with a more vertically developed, robust jawbone, often linked to proper oral posture.
- Chin Projection (Pogonion): The forward-most point of the chin. A greater projection relative to the forehead and nose suggests a more developed chin bone (menton).
While you cannot measure the angle directly, you can use a mirror and a straight edge to visually assess the sharpness of your jaw angle.
For the width, a simple tailor’s tape measure or a large caliper can provide a reasonable estimate of the bigonial distance.
B. Zygomatic Width (Cheekbone Mass)
The prominence of the cheekbones is a key indicator of zygomatic bone mass.
The Bizygomatic Width (the distance between the most prominent points of the cheekbones) is the standard measurement.
A greater bizygomatic width suggests a larger, more projected zygomatic arch, which contributes significantly to midface volume and definition.
This measurement, combined with the bigonial width, forms the basis of the Facial Width-to-Height Ratio (fWHR), which is a proxy for overall facial robustness Facial Anthropometry and Aesthetics.
Method 2: The Functional Proxy—Assessing Muscle and Load 🏋️
Since bone responds to mechanical load, the strength and function of your facial muscles can serve as an indirect measure of the load being placed on your facial bones.
A stronger masseter muscle, for example, suggests a greater biting force, which in turn stimulates the jawbone to maintain or increase its density.
A. Masseter Muscle Hypertrophy (Jaw Muscle Size)
The masseter muscle is the primary muscle of mastication (chewing) and is located at the angle of the jaw.
To assess its size, clench your teeth firmly and feel the muscle bulge at the back of your jaw.
A larger, more developed masseter muscle is a sign of frequent, strong use, which is beneficial for jawbone density.
While not a direct measure of bone mass, a strong masseter is a functional proxy for a well-loaded and likely denser jawbone.
B. Oral Posture and Tongue Strength
Proper oral posture, often associated with the practice of “mewing,” involves resting the entire tongue against the roof of the mouth.
This posture exerts a gentle, constant upward force on the maxilla (upper jaw), which is theorized to stimulate bone growth and maintenance over time.
While the long-term effects on adult bone mass are debated, the ability to maintain this posture comfortably is an indicator of correct muscle function, which supports the craniofacial structure.
The functional proxy relies on the principle that use it or lose it applies directly to bone tissue.
Method 3: The Symptomatic Proxy—Looking for Signs of Loss 📉
In adults, a decrease in facial bone mass is often accompanied by visible aesthetic changes and dental symptoms.
Observing these changes can serve as a symptomatic proxy for bone loss.
- Recession of the Chin and Jawline: As the mandible bone resorbs, the chin can appear more recessed, and the jawline loses its sharp definition. This is a common sign of age-related bone loss in the lower face.
- Midface Flattening: Resorption of the maxilla and zygomatic bones leads to a loss of support for the soft tissues, resulting in a flattened midface and the appearance of deeper nasolabial folds.
- Dental Changes: Bone loss in the alveolar ridge (the part of the jawbone that holds the teeth) can lead to loose teeth, gum recession, and changes in bite alignment.
- Tooth Loss: The most severe indicator of jawbone atrophy is tooth loss, which dramatically accelerates bone resorption due to the complete lack of mechanical stimulation.
If you notice a significant change in your facial profile or dental stability, it is a strong signal that your facial bone mass may be decreasing, and a professional consultation is warranted.
The Role of Nutrition and Lifestyle in Bone Mass 🥗
Maintaining facial bone mass is a proactive process that is heavily influenced by diet and lifestyle.
The most critical nutritional factors are the synergistic trio of Calcium, Vitamin D3, and Vitamin K2.
| Factor | Role in Facial Bone Health | Home Assessment/Action |
|---|---|---|
| Vitamin D3 | Essential for calcium absorption from the gut. | Monitor sun exposure; consider blood test for deficiency. |
| Vitamin K2 | Directs calcium into bone tissue (Osteocalcin activation). | Assess dietary intake of K2-rich foods (Nattō, grass-fed dairy). |
| Mechanical Load | Stimulates bone remodeling via Wolff’s Law. | Ensure nasal breathing, proper tongue posture, and a diet that requires chewing. |
| Hormonal Balance | Hormones (e.g., estrogen, testosterone) regulate bone turnover. | Monitor sleep, stress, and exercise levels (proxies for hormonal health). |
Beyond nutrition, lifestyle factors such as chronic stress, lack of sleep, and excessive alcohol consumption can negatively impact bone density by disrupting hormonal balance.
A holistic approach to health is the best long-term strategy for maintaining a robust facial skeleton.
The Limits of At-Home Measurement 🛑
It is critical to emphasize that no at-home method can accurately measure bone mineral density (BMD) or bone mass.
The gold standard remains the Dual-Energy X-Ray Absorptiometry (DEXA) scan, which is a medical procedure.
The methods described here are proxies—they allow you to gauge the potential for strong bone mass based on external structure and functional habits.
They are tools for self-awareness and motivation, not clinical diagnosis.
If you have a medical concern about bone loss, especially if you have a history of osteoporosis or unexplained dental issues, you must consult a physician or dentist for professional imaging and testing.
However, by consistently monitoring your facial dimensions and ensuring optimal functional habits, you are taking proactive steps to support your craniofacial health.
The goal of at-home assessment is not precision, but awareness of the factors that contribute to a strong facial foundation.
Conclusion: Empowering Your Facial Structure 💯
The quest to measure facial bone mass at home is a testament to the growing awareness of the importance of skeletal health in aesthetics. 💡
While you cannot perform a DEXA scan in your bathroom, you can use anthropometric measurements, functional assessments, and symptomatic observation to gain a powerful, indirect understanding of your facial bone health.
A strong, well-defined jawline and prominent cheekbones are not just genetic gifts; they are often the result of proper growth, correct oral posture, and lifelong nutritional support.
By focusing on the principles of Wolff’s Law—loading your bones through proper chewing and posture—and ensuring a diet rich in D3 and K2, you are actively participating in the maintenance of your facial skeleton.
Use these at-home methods as a starting point for a deeper commitment to your craniofacial health.
A robust facial structure is the ultimate anti-aging secret, providing the support necessary for a youthful and defined appearance for decades to come.
https://youtu.be/YOUTUBE_URL_1
https://youtu.be/YOUTUBE_URL_2
https://youtu.be/YOUTUBE_URL_3
Key Takeaways and Actionable Steps ✅
- Indirect Measurement: Use a ruler or caliper to measure Bigonial Width and Bizygomatic Width as proxies for bone mass.
- Functional Assessment: Check for a strong masseter muscle and the ability to maintain proper tongue posture (mewing).
- Nutritional Support: Ensure adequate intake of Vitamin D3 and K2, the essential co-factors for calcium integration into bone.
- Symptom Check: Be aware of signs of bone loss, such as chin recession, midface flattening, or loose teeth.
- Professional Consultation: For clinical diagnosis, a DEXA scan or CBCT is required; at-home methods are for awareness only.
Your facial bone mass is a reflection of your overall health—invest in it wisely.
Start measuring and optimizing today! 📌